Power of Partnership: Enhancing Antimicrobial Stewardship Capacity at Makerere University Health Services
5 April 2022

Antimicrobial resistance is no longer a silent pandemic. Through the Commonwealth Partnerships for Antimicrobial Stewardship Scheme, Makerere University Health Services in Uganda is working in partnership with Buckinghamshire Healthcare NHS Trust in the UK to tackle AMR before it is too late.
The challenge
Antimicrobial resistance (AMR) is not a silent pandemic. We know from Murray and colleagues that AMR caused an estimated 1.27 million deaths and it was related to a further 4.97 million in 2019. Until now, this is the most comprehensive estimate of the AMR burden. We also know the leading pathogens that cause death associated with resistance. These are Escherichia coli, Staphylococcus aureus, Klebsiella pneumoniae, Streptococcus pneumoniae, Acinetobacter baumannii, and Pseudomonas aeruginosa. Of these, only Streptococcus pneumoniae has an effective vaccine. However, there lies a problem of underinvestment in the efforts to curtail the burden of these infections. Reliable water and sanitation, public health and hospital hygiene which are important ways to prevent drug-resistant infections have been under emphasized in many low- and middle-income countries (LMICs). Even adequate access to effective antimicrobials for treatable illnesses is often not given the attention it deserves. That is why lower respiratory infections stood out as the most vicious infectious syndrome, accounting for more than 1.5 million deaths caused by resistance in a recent study.
Additionally, sub–Saharan Africa (SSA) had a disproportionately higher AMR burden than the rest of the world. In 2019, an estimated 255,000 deaths were due to resistance in the 46 countries surveyed. Taking a simple average, it implies that each country including Uganda lost at least 5,544 lives that year, and thus registered 15 deaths per day due to resistance. This message gets clearer when you think that each of the 15 regional referral hospitals in Uganda lost one life each day to AMR, not forgetting that many more deaths from other causes had AMR as an underlying problem. It is also higher than deaths due to COVID-19 over the past two years in Uganda. Therefore, we need to pick ourselves up and double our efforts against AMR before it is too late.
Commonwealth Partnership of Antimicrobial Stewardship (CwPAMS) scheme
Under the Commonwealth Partnerships for Antimicrobial Stewardship (CwPAMS) scheme, the Tropical Health Education Trust (THET) and the Commonwealth Pharmacists Association came together to curtail AMR. Through the health partnership model, CwPAMS aims to improve awareness, detection and monitoring of resistant infections at the hospital level, taking measures to improve infection prevention, and control and preserve the effectiveness of antibiotics by ensuring judicious use. Since March 2019, four Ugandan regional referral hospitals namely, Jinja, Entebbe, Fort Portal, St Mary’s Hospital Lacor and one national referral hospital (Kawempe National Referral Hospital) have been supported by the CwPAMS scheme. A sixth hospital based at Makerere University joined the scheme in November 2021.
Simply put, in a health partnership, two institutions from different countries mutually agree to improve health and health services based on ideas of co-development, reciprocal learning and mutual benefits over the long term. In our case, the Buckinghamshire Healthcare NHS Trust (BHT) in the United Kingdom partnered with Makerere University Health Services (MakHS) in Uganda.
Sustainable Centre of Excellence for Integrated Antimicrobial Stewardship and Infection Prevention and Control (SIAMS-IPC)
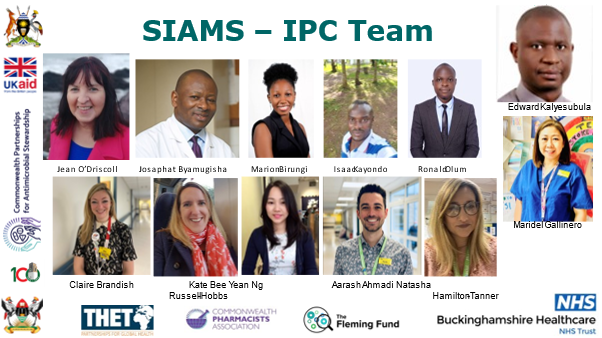
The partnership is operationalized by a multi-disciplinary team of healthcare professionals from both health partners. They include Mrs Claire Brandish, lead antimicrobial pharmacist, Ms Kate Russell-Hobbs, a senior clinical pharmacist for HIV and infectious diseases, Dr Jean O’Driscoll, Consultant Microbiologist, Natasha Hamilton-Tanner, Intensive Care Pharmacist, Aarash Ahmadi, Antimicrobial Pharmacist and Maridel Gallinero, Sister for Intensive Care all based at BHT and Ms Bee Yean Ng, an Antimicrobial Pharmacist at Oxford University Hospital. The MakHS team has Dr Freddy Eric Kitutu, a senior lecturer of Health Systems Pharmacy in the Department of Pharmacy and Acting Dean of the School of Health Sciences, Dr Josephat Byamugisha, a professor of Obstetrics and Gynaecology and Director of MakHS, Mr Isaac Kayondo, the hospital pharmacist, Dr Allan Kalyesubula, a lecturer and dental surgeon, Eunice Namubiru, a Nursing Officer, Dr Ronald Olum, an intern medical doctor and Ms Marion Birungi, the project coordinator. Together, they have created an effective, collaborative and productive team that is working towards a common goal of establishing a Sustainable center for integrated AntiMicrobial Stewardship and Infection Prevention and Control (SIAMS-IPC) at MakHS.
Achievements so far
The SiAMS-IPC team has supported MakHS to formulate a Medicines Therapeutic Committee (MTC) with 23 members, representative in character and gender and balanced with student representation. The MTC is the vehicle through which AMS and IPC practices will be implemented at the hospital. They have also co-opted pharmacovigilance and health commodity supply chain functions as stipulated in the national guidelines. The MTC has comprehensive terms of reference that are a combination of roles and responsibilities of the four constituent sub committees – AMS, IPC, pharmacovigilance and health commodity supply chain. They have been oriented on how the MTC functions to achieve the intended AMS and IPC outcomes, i.e., “to promote and monitor the judicious use of antimicrobials to preserve future effectiveness” and “to prevent patients and healthcare workers from being colonized with bacteria or getting infections”, respectively. Two intense, hybrid (face to face and virtual combination) interactive capacity building sessions have been delivered to fifty healthcare workers inclusive of the facilitators. The health worker participants consisted of consultant radiologists, gynaecologists, nursing officers, medical officers, enrolled nurses, laboratory technicians, laboratory technologists, pharmacy technicians, pharmacists, optometrists, records officer, dental surgeons, hospital cleaners, accountant, office messenger and other support staff.
These have imparted knowledge and skills on implications of gender and social inclusion in addressing AMR, use of guidelines for AMS and IPC and supplemented by the WHO competency framework for healthcare workers’ education and training on AMR, WHO Access, Watch and Reserve (AWaRe) classification antibiotics, hand hygiene, utilisation of Personal Protective Equipment (PPE)and Aseptic Non-Touch Technique (ANTT). The capacity building deployed innovative teaching methods including games and technologies such as use of the CwPAMS antimicrobial prescribing app (CwPAMS MicroGuide®) which hosts the Ugandan Clinical Guidelines, playing the CwPAMS AMS game®, and Glo Germ experiment to illustrate proper handwashing and the balloon experiment (e-Bug) to illustrate the phenomenon of resistance. Mentimeter was also successfully used to maximise interaction among the participants and with the facilitators who were connecting via Zoom. The SIAMS-IPC team has also effectively used social media to disseminate information on its activities. This has been majorly via Twitter. Over the past five months, the Twitter posts by SIAMS-IPC team have in total generated over 100,000 impressions.
One participants of the workshop gave the following feedback on the workshops:
“This training improved my understanding of the burden of antimicrobial resistance and how to prevent it. I also learnt to prescribe antibiotics rationally by utilising appropriate diagnostics and the prescription guidelines. I am ready to practice the skills I learnt, as well as discussing them with my colleagues who did not attend this training” – Intern dental surgeon volunteering with the MakHS
From a UK perspective, SiAMS-IPC project has provided members of the group a unique opportunity to understand how hospital committees such as the MTC are formulated and what clinical governance arrangements need to be established in order to ensure representation, ownership and empowerment. The workshops provided a forum in which case studies could be discussed to understand current practices, review the guideline recommendations and consider if new evidence has come to light that may require a change. An example of this is the dosing of ceftriaxone for gonorrhoea due to resistance. It was also noted that generating healthy conversations with patients to enable them to weigh up the risks and benefits of taking antibiotics and become part of the shared decision-making process is a challenge in both the UK and Uganda. In fact, recent study by Olum and colleagues showed that only 1 in 10 Uganda patients participate in shared decision making during their healthcare. It important to provide sign posting to patients if antibiotics are not deemed necessary, but they should feel able to re-present if they become sicker or do not improve.
Finally, it is imperative that you and I do everything in our capacities to fight this overlooked pandemic by ensuring appropriate infection control and prevention practices, and rational drug prescriptions during our practice. As patients, we can contribute by avoiding self-medication, preventing infections by proper sanitation, hygiene, and vaccination, and following the advice of healthcare workers when we seek care. Let us work together to fight antimicrobial resistance!
– SiAMS-IPC team: Freddy Eric Kitutu, Claire Brandish, Ronald Olum, Kate Russell Hobbs Jean O’Driscoll, Bee Yean Ng Natasha Hamilton-Tanner, Aarash Ahmadi, Maridel Gallinero, Isaac Kayondo, Allan Kalyesubula, Eunice Namubiru, Marion Birungi, and Josaphat Byamugisha
References
Antimicrobial Resistance Collaborators; Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis; Lancet. 2022; (published online Jan 20.); https://doi.org/10.1016/S0140-6736(21)02724-0
THE HEALTH PARTNERS
Buckinghamshire Healthcare NHS Trust (BHT) is a major provider of integrated hospital and community services for people living in Buckinghamshire and the surrounding areas. It provides care to over half a million patients every year. It has over 6,000 highly trained clinical staff who include doctors, nurses, pharmacists, midwives, health visitors, therapists, and healthcare scientists. It is nationally recognised for urology and skin cancer services and are a regional specialist centre for burns care, plastic surgery, stroke and cardiac services and dermatology. BHT also provide specialist spinal services at the world renowned National Spinal Injuries Centre for patients from across England and internationally.
Makerere University Health Services (MakHS) is the umbrella directorate that hosts health services offered by Makerere University Hospital, the Dental Hospital, the Academic Vision Center and satellite clinics at Kabanyolo and Jinja campuses. Its vision is to be a leading healthcare organization, nationally and internationally, improving health outcomes through research, training, collaboration and innovation. And its mission is to provide the best care to every client through its personal and shared commitment to excellence in clinical practice, education, research and innovation, while fostering our partnership with Makerere University College of Health Sciences. The main Makerere University Hospital started in 1978 and it is located on Bativa Road, off Gaddafi Road in Wandegeya, Kampala, Uganda. It provides healthcare to the Makerere University community including faculty, students and the general public who are the relevant stakeholders. It is managed by Makerere University College of Health Sciences (MakCHS) and supported by faculty from the diverse range of departments at MakCHS. More information is available here.